Last updated on October 21st, 2025 at 02:38 pm
Bloating is one of the most common, and often most distressing, physical symptoms people experience during anorexia recovery. After months or even years of restricting food, the digestive system needs time to heal, which can make even small amounts of food feel overwhelming.
The uncomfortable fullness, stomach distension, and gas aren’t just physical hurdles; they can also intensify body image struggles and fuel doubts about recovery. While bloating can feel scary, it’s actually a sign that your body is working hard to repair itself.
This article will explore why bloating happens, how long it lasts, potential risks, and how to ease discomfort to make the process a little easier.
What is Bloating In Anorexia
Bloating in anorexia refers to the uncomfortable swelling, pressure, or distension in the stomach and intestines that often happens when someone with anorexia begins eating more food during recovery. It’s a common digestive response because your body has gone through long periods of restriction, slowing down gut function and reducing the production of important digestive enzymes and stomach acid.
When eating increases again, the digestive system can feel overwhelmed leading to gas buildup, delayed stomach emptying, and a feeling of fullness or tightness in the abdomen.
Normal Eating Disorder Recovery Bloating
In anorexia recovery, bloating typically isn’t a sign that something is “wrong” with your body, it’s usually a sign that your digestive system is restarting, rebalancing, and working to adapt to consistent nourishment again. While it can be uncomfortable (both physically and emotionally), it’s a temporary stage of healing.
Common features include:
- A feeling of fullness or pressure in the stomach, especially after meals
- Visible distension or swelling in the abdomen
- Gas, burping, or increased flatulence
- Temporary constipation or changes in bowel movements
These symptoms usually improve as your digestive system adapts to regular food intake. They’re uncomfortable, but generally not dangerous.
When Anorexia Bloating Might Signal a Medical Issue
While most bloating in recovery is harmless, there are times when it’s important to seek medical support.
Watch out for:
- Severe or sudden abdominal pain that doesn’t improve
- Persistent vomiting or inability to keep food or fluids down
- Blood in stool or vomit
- Fever, chills, or signs of infection
- Extreme constipation lasting more than a few days despite eating and hydrating normally
These can point to complications like refeeding syndrome, bowel obstruction, or other digestive conditions that need medical attention.
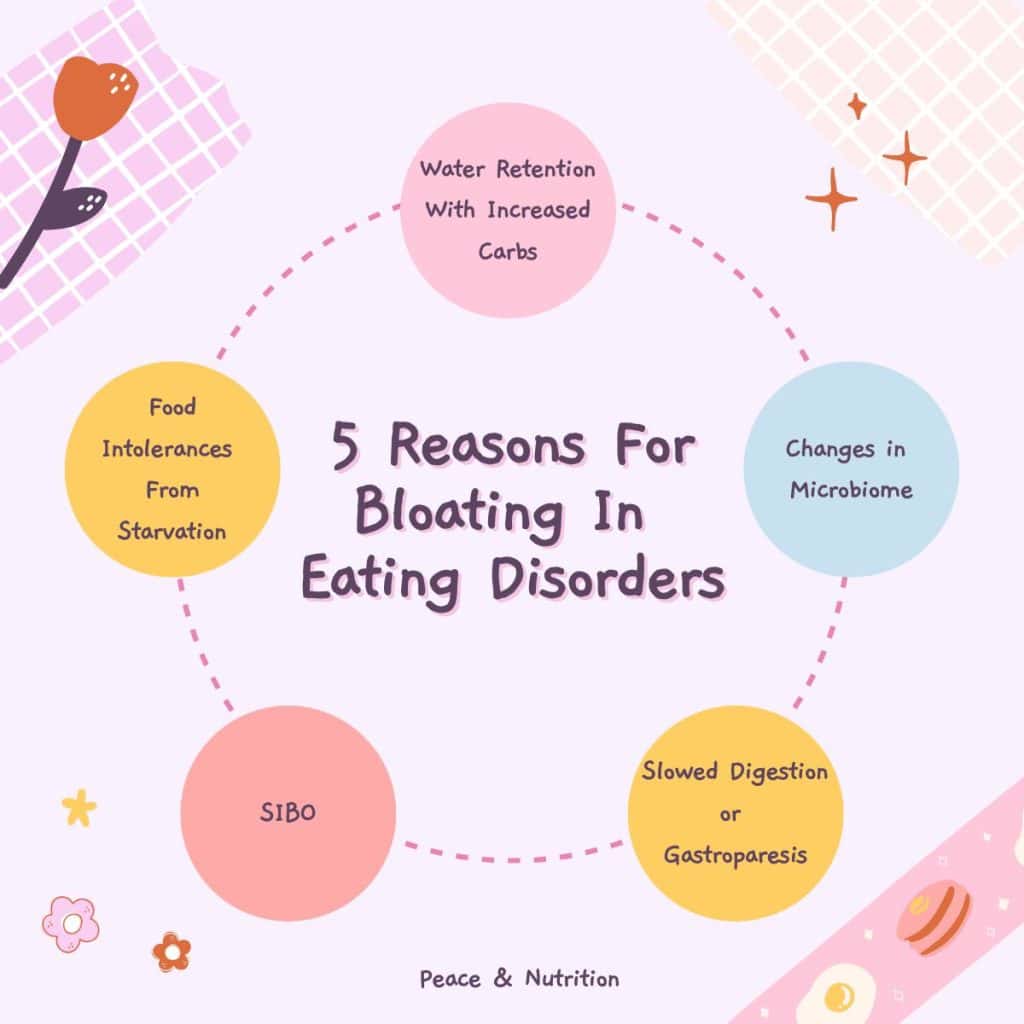
5 Causes of Bloating In Anorexia and Recovery
Slowed Digestion and Gastroparesis
When someone is recovering from anorexia, the digestive system often slows down because the body has been in a state of energy conservation for so long. This slow digestion is sometimes called delayed gastric emptying, and in more severe cases, it can develop into gastroparesis (a condition where the stomach muscles don’t move food along as quickly as they should).
You may also be sitting with the urge to purge or have muscle deterioration from laxative abuse which can make slowed digestion and bloating even more extreme.
When the stomach empties slowly, food and liquid sit in the stomach for longer than usual. This leads to:
- Gas buildup as food ferments
- Pressure and fullness because the stomach feels stretched
- Visible distension
- Feeling full quickly or not having hunger cues
For people in anorexia recovery, this can feel especially uncomfortable because even small meals may trigger a disproportionate sense of fullness and bloating. While slow digestion and gastroparesis are frustrating, they’re usually a result of the body adapting to long-term restriction and often improve with consistent, gentle nourishment over time.
Refeeding and Increased Carbohydrate Intake
During eating disorder recovery, especially in the early stages of refeeding, many people notice that bloating worsens when they start eating more food — particularly carbohydrates. This happens for a few key reasons:
- Glycogen Storage and Water Retention
When you eat carbohydrates, your body breaks them down into glucose for energy.Any extra glucose is stored in the liver and muscles as glycogen.For every gram of glycogen stored, your body holds onto about 3–4 grams of water.This natural process can make you feel puffy, swollen, or bloated, especially in the stomach area.
- Increased Fermentation in the Gut
After restriction, your gut bacteria may be out of balance.A sudden increase in carbs (especially fiber or sugars) can lead to more fermentation by gut bacteria.This produces extra gas, leading to bloating, cramping, and flatulence.
- Digestive System “Reboot”
With consistent nourishment, your digestive system starts working harder and faster again.Early on, it may struggle to handle the volume and variety of carbs, causing temporary discomfort until it adapts.

Food Intolerances and Sensitivities After Restriction
After an eating disorder, many people notice that certain foods seem to cause more bloating, gas, or stomach pain than they used to. This isn’t always a sign of a permanent food intolerance, often, it’s a temporary sensitivity that develops because of how restriction impacts the digestive system.
- Reduced Enzyme Production
Long-term restriction can decrease the body’s production of digestive enzymes (like lactase, which breaks down lactose in dairy). When foods aren’t fully broken down, they ferment in the gut, leading to gas and bloating. - Changes in Gut Lining and Motility
Undernourishment can thin the gut lining and slow intestinal movement.
This makes the gut more sensitive to foods like dairy, wheat, beans, or high-fiber items. - Altered Gut Microbiome
Restriction and malnutrition disrupt the balance of healthy gut bacteria.Reintroducing certain foods can trigger gas and bloating until the microbiome stabilizes. - Heightened Gut Sensitivity (Visceral Hypersensitivity)
After an eating disorder, the digestive system can become more reactive.
Even normal amounts of gas or pressure may feel painful or extreme, making food reactions seem more severe.
Hormonal Changes and Fluid Retention
Hormonal changes are another reason bloating is so common during eating disorder recovery. When the body has been undernourished, levels of key hormones like estrogen, progesterone, cortisol, and insulin are often disrupted. As regular nourishment returns, these hormones begin to rebalance, but the transition period can come with uncomfortable side effects, including fluid retention and bloating.
Estrogen and progesterone, in particular, influence how much water the body holds onto. As these hormones normalize, especially if menstrual cycles return, it’s common to experience water retention around the abdomen, hips, and legs.
Cortisol, the body’s stress hormone, can also affect fluid balance. During recovery, stress levels and cortisol fluctuations may cause the body to temporarily cling to extra water, creating a swollen or puffy feeling.

Small Intestinal Bacterial Overgrowth (SIBO)
Another possible contributor to bloating in eating disorder (ED) recovery is small intestinal bacterial overgrowth (SIBO). SIBO happens when too many bacteria grow in the small intestine, where there normally should be only a small amount. These bacteria ferment food before it can be properly digested and absorbed, producing excess gas, resulting in bloating, abdominal distension, cramping, and sometimes diarrhea or constipation.
Eating disorders, especially those that involve long-term restriction or purging, can increase the risk of SIBO. Malnutrition and slowed digestion weaken the muscles of the gut and reduce stomach acid production, both of which normally help keep bacteria in balance. When digestion slows down, food lingers in the small intestine longer, giving bacteria more opportunity to multiply.
This overgrowth can make bloating in recovery more severe, persistent, and painful than the “usual” temporary bloating that comes from refeeding or food sensitivities.
How Ease Discomfort From Anorexia Bloating
Bloating in recovery can be uncomfortable and sometimes emotionally triggering, but there are gentle strategies that can help your digestive system adjust and relieve discomfort.
Ease discomfort from bloating in eating disorder recovery by:
- Eating smaller, more frequent meals to give your digestive system time to adjust.
- Chewing food thoroughly to aid digestion and reduce swallowed air.
- Staying hydrated with water or gentle herbal teas to support gut function.
- Incorporating gentle movement like walking or yoga, to stimulate digestion.
- Using warm compresses or heating pads on the abdomen to relax stomach muscles.
- Limiting carbonated drinks and chewing gum to reduce excess gas.
- Adding fiber gradually instead of all at once to prevent sudden bloating.
- Practicing stress management such as mindfulness, deep breathing, or meditation.
- Attempting to use the bathroom at the same time each day and use a squatty potty
- Being patient with your body bloating is usually temporary and a sign of healing.
- I Wish I Had More Control With Food - November 18, 2025
- The Fattest Person in the Room - November 18, 2025
- 10 Tips To Cope With Bad Body Image Days - September 29, 2025